Case Study: Patient Exposed to Mold
Let me be frank. There’s not a day in my practice when I don’t see a patient with multiple health diagnoses. It’s very common, but not overwhelming when you understand the underlying mechanisms of what’s going on. Let me tell you about a recent patient named Susan.
Susan came to see me with a laundry list of ailments. By 38, she had amassed the following conditions: irritable bowel syndrome (IBS), chronic headaches, allergies, severe weight gain, swelling of the feet, autism with generalized anxiety; and muscular dystrophy.
This is not normal at the young age of 38. As a mental health advocate, Susan knew something was not right with her body because she wasn’t as emotionally engaged as she used to be. She felt “off”, and she wanted to know what she could do to live a relatively pain-free existence and be free from her anxious tendencies and persistent allergies. I had a hunch that something in her diet was not working for her.
After reviewing her commonly consumed foods, I noticed a majority of her diet included GMO crops (i.e. wheat, corn, soy), animal proteins (most often fed GMO crops), alcohol, coffee, dried fruit and fruit juices. This gave me a clear indication of what I needed to look for.
I assessed Susan’s environmental toxicant exposure and over toxin load. While similar in their toxic effects to the human frame, it’s important to distinguish the difference between the two terms when talking to your healthcare provider. A toxin is something natural, like snakes’ venom or mold. A toxicant is something man-made, like pesticides or industrial pollution, that is ultimately released into the environment and finds its way inside of our bodies. Susan’s levels of toxins and toxicants were off the charts because of her diet.
While her RoundUp level (a toxicant) was noticeable, I was more concerned about the toxins released from various mold found inside Susan. More on this below.
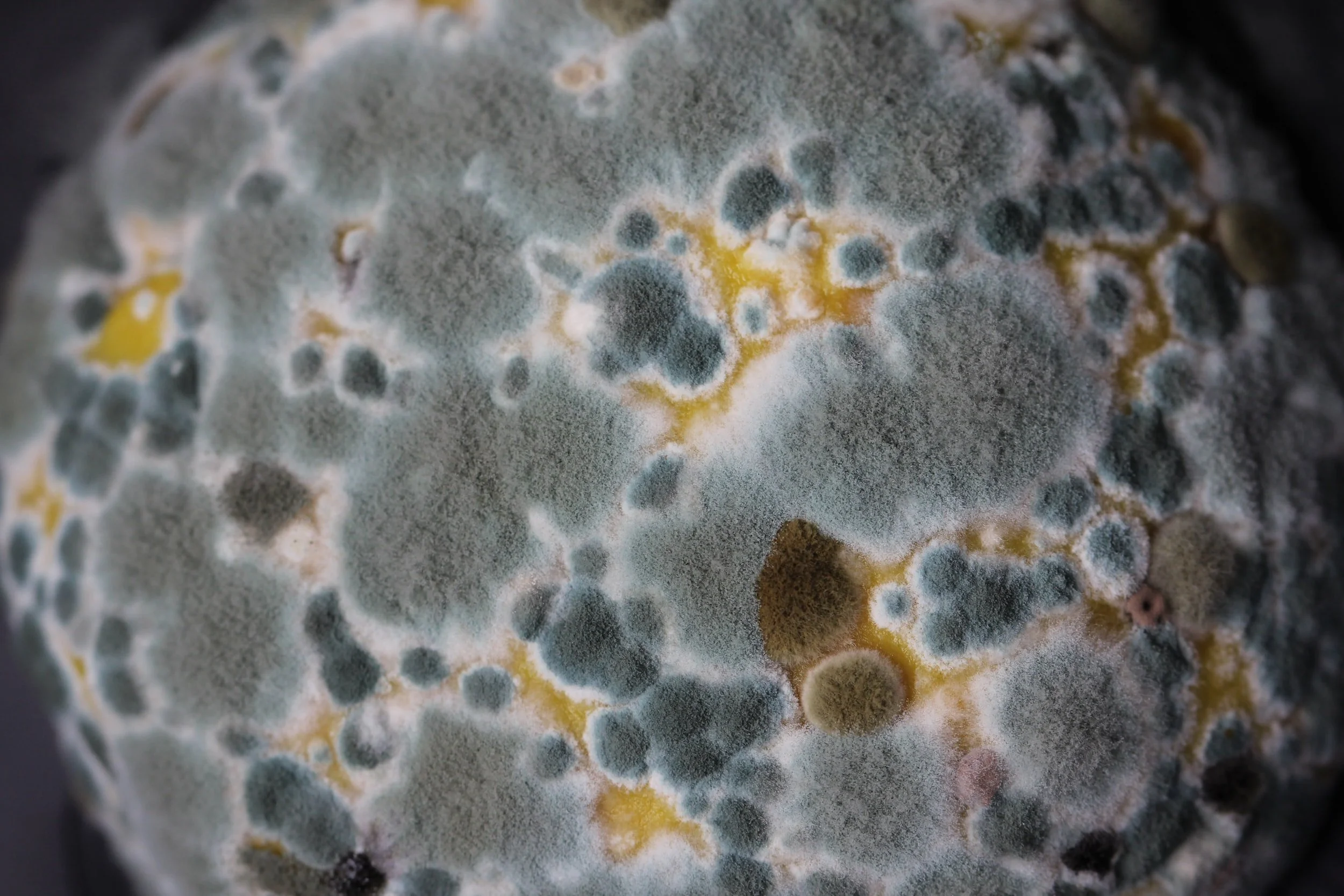
But first: when I was in school, mold exposure was only discussed in the context of indoor and outdoor environments. It was understood that molds grow best in warm and wet conditions. Common indoor molds to consider were Aspergillus, Alternaria, Cladosporium and Penicillium. We didn’t realize is most heavily present in many foods we often consume and does not get killed with heating, freezing, pasteurizing, roasting (aka., cooking). Mold has easily survive in the most harsh and dry conditions.
Ubiquitous molds will produce mycotoxins (i.e. mold + toxin), very toxic molecules which make people very ill over time. For Susan, she had extremely high levels of Ochratoxin A, a mycotoxin produced by Aspergillus and Penicillium mold species. These molds are heavily grown on economically important crops and food products heavily consumed in the U.S. (i.e, wheat, corn, soy, animal protein, dried fruit, fruit juice, coffee, alcohol). Mold toxicity illness is associated with various chronic health problems, including autoimmune disorders, liver and kidney disease, autism, chronic fatigue, and certain cancers.
Very few, if any, conventional doctors test for Ochratoxin A, which is alarming since the International Agency for Research on Cancer hasclassified this mycotoxin as a possible human carcinogen (i.e. group 2B carcinogen).
For Susan, it was clear to me that her food choices ultimately lead to an insidious overconsumption of Ochratoxin A, and subsequently gave way to a wide array of symptoms. The most common food sources of molds include:
- Grains such as wheat, corn, and/or soy
- Animal protein since they are fed wheat, corn, or soy at some point of their life. This includes all meats, dairy products, eggs, poultry, and fish.
- Coffee
- Wine
- Peanuts
- Fruit juice (ie., berries, grapes, citrus)
- Dried fruit
The first step in Susan’s mold treatment was the reduction in the commonly contaminated foods that were causing her symptoms. Of course, there are other treatments, like antifungal medication, antioxidant therapy, sauna detoxification, and botanical supplements, but I started simply with making significant dietary changes. This would have the greatest impact.
In less than 1 month, Susan has been feeling more alive, emotionally engaged, physically stronger, and more stable than she can remember. We are continuing to work with these changes in addition to diving deeper into mindfulness, breathing practices, and supplementation for cellular support.
By avoiding large dinners, animal proteins, and GMO crops, while optimizing Susan’s hydration, her allergies are dramatically lessening each week.
What you should know about Ochratoxin A
It's a chemical byproduct released from molds in the Aspergillus and Penicillium families that has nephrotoxic, immunotoxic, neurotoxic, and carcinogenic properties.
- Exposure can occur from water damaged buildings, inhalation of other water damaged spaces, or through contaminated foods like cereals, grape juices, dairy, wine, dried vine fruit, and coffee.
- If ingested or inhaled, exposure can lead to kidney disease and adverse neurological effects; Ochratoxin A is thought to give rise to significant oxidative damage to multiple brain regions, thus leading to its adverse effects on the central nervous system (CNS).
- Dopamine levels in the CNS of mice have been found to decrease after exposure to Ochratoxin A.
- It's hypothesized that Ochratoxin A may be associated with the eventual development of neurodegenerative disorders like Alzheimer's and Parkinson's disease.
- Treatment should be primarily focused on removing all sources of exposure.
- Antioxidants like vitamin A, C, E, and selenium are particularly beneficial antioxidants due to their ability to serve as superoxide anion scavengers.
- Other antioxidants to decrease oxidative effects are N-acetylcysteine (NAC), rosmarinic acid, and glutathione alone (or in combination).
- There is anecdotal evidence that sauna therapy can shift the excretion of ochratoxin A into to sweat; however, use of sauna needs to be very carefully monitored, especially on initiation.
AUTHOR
Dr. Payal Bhandari M.D. is one of U.S.'s top leading integrative functional medical physicians and the founder of SF Advanced Health. She combines the best in Eastern and Western Medicine to understand the root causes of diseases and provide patients with personalized treatment plans that quickly deliver effective results. Dr. Bhandari specializes in cell function to understand how the whole body works. Dr. Bhandari received her Bachelor of Arts degree in biology in 1997 and Doctor of Medicine degree in 2001 from West Virginia University. She the completed her Family Medicine residency in 2004 from the University of Massachusetts and joined a family medicine practice in 2005 which was eventually nationally recognized as San Francisco’s 1st patient-centered medical home. To learn more, go to www.sfadvancedhealth.com.